How Syounaa Socks Help With Diabetic Neuropathy
Syounaa Diabetic socks are designed for diabetic patients; particularly those suffering from peripheral diabetic neuropathy. It provides your feet with much-needed care so that you can carry out your daily activities with ease. Our socks are designed to provide patients with comfort and stability that is essential for your routine.
What is Diabetic Neuropathy?
Dr. Paul S., a professor of Surgery in Stanford University School of Medicine, describes diabetic neuropathy as, ‘a form of nerve damage that results from the effects of high of high blood sugar levels upon nerve fibers throughout the body.’ It can occur to both Type 1 and Type 2 diabetic patients and once diagnose, it is difficult to reverse the effects of this condition.
However, with proper care and treatment, we can slow down the damage caused by Diabetic Neuropathy.

What Causes Diabetic Neuropathy?
We have a complex nervous system that allows us to carry on with day to day actions. Movement, muscle contraction and involuntary actions are largely controlled by our nervous system. The nervous system is divided into three distinct sections – autonomic, sensory and motor. The autonomic nervous system refers to the involuntary muscular activities like our heartbeat and muscle movements that digest food in the stomach and small intestine. The sensory nervous system sends signals of touch, temperature, and pain to our brain and the motor system signals the brain to contract muscles when needed. Diabetic Neuropathy is a condition that leads to the damage of the nervous system because of the high glucose content in our bloodstream.
The increased blood glucose causes our blood vessels to narrow. When vital blood vessels, responsible for supplying oxygen to the nervous system, narrows, we see a reduced supply of oxygen to the nervous system. This not only makes the affected nerve perform poorly but the organ or muscle controlled by the nerve cannot function as well as it used to. Research shows that more than 60 % diabetic patients get diabetic neuropathy at a later point in their life. It is a gradual deterioration of the nervous system, which is why patients often get accustomed to the initial stages of this condition.
Types Of Diabetic Neuropathy
There are a few different kinds of diabetic neuropathy. They vary slightly from each other and are named depending on where and how they occur.
Proximal Neuropathy
Proximal Neuropathy largely affects the nerves that supply oxygen to our muscles. It usually affects the muscles in our hips and legs, particularly our thighs and buttocks. Patients with proximal neuropathy often experience a sharp pain from the lower back to the ends of their feet.
It is the second most common kind of neuropathy and largely affects older diabetic people or people who have had diabetes for more than 20 years. It is also one of the few kinds of diabetic neuropathy that may reduce with treatment.
Autonomic Neuropathy
As the name may suggest, autonomic neuropathy affects the autonomous nervous system. These are the nerves responsible for maintaining homeostasis or maintaining the body in its normal balanced state. So, your optic nerve allows us to see, intestine nerves help the digestive system work normally, nerves to our heart supply oxygen to our heart so that it can maintain a steady heartbeat, and so on. All these bodily processes take place without us consciously thinking about it. When diabetes affects the autonomic nervous system, it disrupts our homeostasis. So, autonomic neuropathic patients may have trouble hearing, seeing, may face constipation, an irregular heartbeat and so on. The effects and severity of autonomic neuropathy depends on the specific autonomic nerve it has damaged.
Focal Neuropathy
Unlike all other kinds of neuropathy, focal neuropathy affects a specific nerve which is why it is also called mononeuropathy whereas the other forms of neuropathy are referred to as ‘polyneuropathy’. It largely affects the nerves leading to our brain and eyes but it can also affect our legs and lower body. The symptoms caused by focal neuropathy, affecting the legs is very different from proximal neuropathy. While proximal neuropathy causes a shooting pain from the hip and below, focal neuropathy causes pain only in particular parts of the leg.
Peripheral Neuropathy
Peripheral Neuropathy is one of the most common types of Diabetic Neuropathy. It affects the peripheral, or outer parts, of your body, like our arms, legs, hands, and feet. The nerve ending on our hands and feet are the longest nerves in our body. These nerves, especially the ones leading to our feet branch out from our lower back and supply oxygen to both our feet. Since they are the longest nerves in our body they are most susceptible to nerve damage.
Many describe peripheral neuropathy as pain, numbness and a tingling sensation. Because of the numbing sensation, some patients are unable to feel cuts, bruises and foot sores until it has developed into an infection. In worst cases, unattended wounds of a peripheral neuropathic patient have led to amputations.
How It Affects Daily Life
Diabetic Neuropathy affects different diabetic individuals at any age. Around 60 to 70 percent of diabetes patients have mild to severe forms of diabetic neuropathy. The milder forms can often go unnoticed however severe cases can not only affect your daily activities but may impair you, and force you to take external assistance.
In October 2011 Tracy Neithercott wrote an article for Diabetes Forecast, where she documented the conditions of type 1 diabetic patient with severe diabetic neuropathy – Lee Nevitt. Lee Nevitt describes diabetic neuropathy as ‘hell’. His feet feel sensitive even on the slightest contact with the blanket. He says that touching his feet during this time is unthinkable. Nevitt describes the pain as having a burning sensation and sometimes feeling electric shocks around the feet.
Lee Nevitt’s diabetic neuropathy has led to hypersensitivity of the nervous system which makes his feet sensitive to the slightest touch. Diabetic neuropathy can also have complete opposite symptoms. You may feel numbness around your feet and arms. Pyllis Bear, a peripheral neuropathy patient, describes it as ‘feeling disconnected from the feet.’ Both hypersensitivity and insensitivity are serious symptoms. If you are a diabetic neuropathic patient, who notices insensitivity of certain parts of the legs, you must not ignore cuts; even those that seem completely harmless.
How To Diagnose Diabetic Neuropathy
Never ignore symptoms of pain, numbness, loss of sensation on any part of your body. Frequent visits to the clinic is a must. Below are some more symptoms of diabetic neuropathy:
Symptoms:
- Numbness or extreme pain
- Muscle weakness or shrinkage
- Gradual loss of sensation at the tips of our fingers and the ends of our feet
- Difficulty co-ordination and walking
- Dizziness upon standing
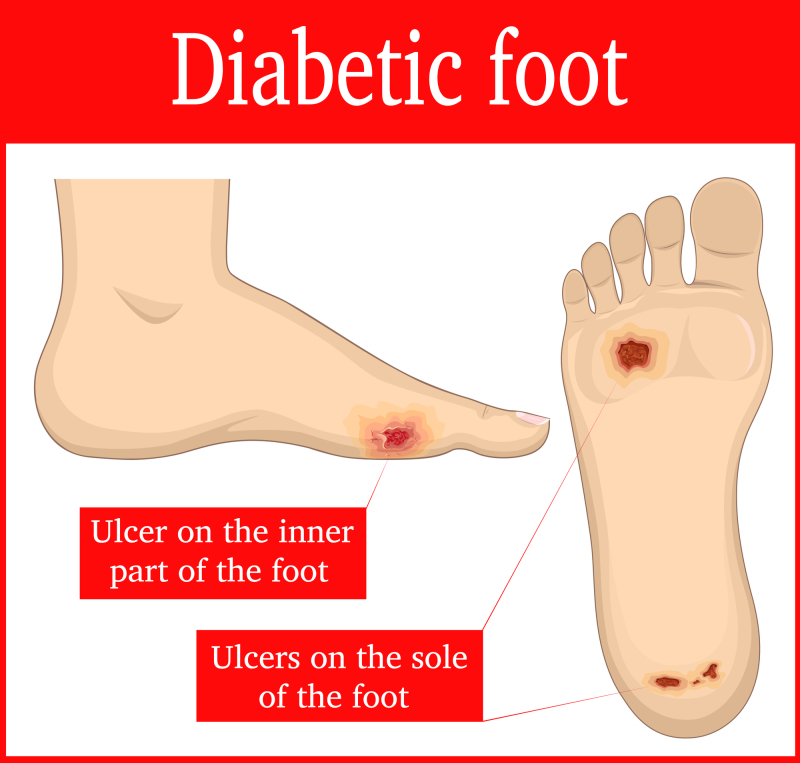
- Foot ulcers
- Frequent Skin Infection
- A tingling or numbing sensation around our arms and legs
- Not being able to feel cuts and scars around our feet
Visit your doctor if you have any of the above symptoms because the longer you wait, the worse it gets. Your doctor will first evaluate your diabetic history hear your symptoms and check your muscular strength, reflexes, and sensitivity to touch.
Doctors start by checking your skin for cracked surfaces, blisters, soars and bone, and joint problems. After a thorough understanding, they may conduct different tests according to your symptoms. Below are a few tests that they may perform to get a better understanding of the severity of your diabetic neuropathy.
Filament Test
The filament or monofilament test is a non-invasive method of investigation where the doctor uses a 10g monofilament to examine the sensitiveness of your feet. The doctor will use a soft nylon fiber and brush it along the parts of your skin where you claim is sensitive. Since the patient is in a lying position, he/she cannot see the doctor and their foot. This allows the doctor to touch certain parts to the patient’s feet and ask if they feel the filament. Doctors do not apply any pressure on the filament, it is just enough to touch certain points of your feet. The filament test is done to test nine distinct nerve points on the sole of our feet. It is a light touch and is enough for a non-neuropathic patient to feel it but diabetic neuropathic patients often struggle with this experiment.
Quantitative Sensory Testing
Doctors conduct this test if their patients complain about their inability to feel certain temperature changes. In this test, doctors will check how your body responds to vibration and subtle changes in our surrounding temperature. It helps to identify the initial stages of peripheral neuropathy.
Nerve Conduction Studies
This test measure how quickly our arms and legs conduct electric signals. The nerve is stimulated usually with electrode patches that are stuck to your skin. Two electrodes are placed on the skin over your nerve while one stimulates your nerve with a mild electrical impulse and the other makes a record of the change. The electrical activities of your body are then recorded and doctors repeat this process on all the affected nerves.
Electromyography (EMG)
This is often performed with conduction studies. It helps doctors understand if nerve cells are re-generating because in some cases, the neighbouring nerve cells create channels to build connectivity with the parts of muscles that are not receiving oxygen. EMG measures the electrical discharges produced in your muscles.
Autonomic Testing
For those who have symptoms of autonomic neuropathy, there are special tests done to determine the changes in blood pressure while you move and are in different positions. Doctors also check if you sweat normally.
The tests mentioned above help us understand the type of diabetic neuropathy we have and the severity of our condition. It is important as it makes us aware of our condition so that we can take steps to better health.
How To Manage Diabetic Neuropathy
Managing Blood Sugar Levels
As you may know by now, high blood sugar content worsens diabetic neuropathy. The damage is irreversible but we can slow down the process by keeping a constant check on our blood sugar levels. Your doctor will inform you about the number of times you should check your blood sugar throughout the day. Ideally, a diabetic patient must check their blood sugar from 4 – 10 times a day. This differs for type 1 and type 2 diabetic patients.
If you keep a constant watch on blood sugar and ensure that it is in range, you would notice lesser pains on other parts of your body. Not only does this prevent the occurrence of diabetic neuropathy but slows down the process immensely. Medication helps you manage blood sugar but we must take conscious initiatives to ensure that our glycaemic index is on the low. Diet and exercise are the two most important ways by which we can keep this condition under control.
Diet
Diet is one of the most important ways by which you can control diabetic neuropathy, especially if your condition limits you from doing certain exercises. We need to eat what we can digest without producing more glucose than what our body needs.
A diabetic patient may neglect their diet sometimes but when we are diagnosed with diabetic neuropathy, we face the consequences of not eating right. Too much sugar can aggravate our condition and increase sensitivity around our feet.
Simple rules come a long way. Make sure you have enough B12 in your diet. Many older individuals have a B12 deficiency and that lack of it can worsen peripheral neuropathy, so, ensure that you get your B12 levels checked. Include natural B12 sources in your diet or add a supplement if your doctor suggests it.
Go for small portions of lean meat that is easy to digest along with a lot of vegetables for roughage. Diabetic patients avoid food that has more sugar or starch but to maintain a healthy lifestyle, you must reduce your salt, potassium and phosphorus int intake. Food that has a lower glycaemic index are the ones that put less pressure on your kidneys are best for your condition. Choose whole wheat bread and roti (flat Indian bread) instead of the ones made with white flour. Substitute potatoes with sweet potatoes. Choose fibrous fruits and vegetables like carrot, and apple because they help you keep your diabetes under control.
Talk to a dietician before enforcing a strict diet. Every diabetic patient has different affected areas and therefore exhibit different symptoms. Some of us can exercise and therefore are in a better position for a flexible diet while others need to follow a strict diet plan. A dietician can study your medical history, evaluate our current lifestyle and design a diet plan accordingly.
Exercise
Food and exercise are important parts of diabetic neuropathy. Consult your doctor before attempting any exercises to be safe. The main purpose of neuropathy specific exercise is to stimulate blood cells and allow better oxygenation around affected areas. Start by simple stretches around your feet and arms. You can use a sturdy, non-stretchable, band to help you stretch your legs out. Workouts like leg lifts also help build stronger legs and allow better circulation.
As diabetic neuropathy increases slowly, you may struggle to keep your balance and therefore exercises that improve your balance will prolong the conditions from getting worse. Hold a stool for support and slowly raise your body until you are on your toes, hold the position for five seconds and come down slowly on your heal. Make sure the movement is slow and steady to promote blood circulation around the heal area. You can also stand on one leg and swap after equal intervals. Hold on to a stool or wall for better control and slowly increase the difficulty by leaving the wall.
Rolling ankles and wrists both clockwise and anticlockwise direction are also great ways to stimulate blood flow. They are simple exercises that anyone can do. Many diabetic neuropathic patients say they benefit from breathing exercises and yoga. Walking also helps diabetic neuropathic patients but it’s important to consult your doctor before adding a walk in your everyday life. Some patients can walk for hours while others may worsen their condition by walking for more than 30 minutes.
Frequent self-checks
As we discussed earlier, a diabetic neuropathic patient may loose sensations from their feet. This may be the reason for cuts and wounds to go unnoticed. These cuts and wounds can later cause infections or worse, gangrene. It is better to be mindful of the injuries we have. Take out time every day to check for sores, cuts, wounds and foot ulcers. You will not have to spend more than 15 minutes examining your arms, hands, palms, legs, and feet.
Give special attention to your feet as most foot injuries go unnoticed. Examine the heels of your feet and between your fingers. Move your limbs as you examine how well you can feel your feet. For better health, do a thorough check-up with your doctor at least once every year.
Maintain hygiene and moisture levels, especially around your feet
Research shows that almost 85% of foot amputations have occurred because of untreated foot ulcers. But foot ulcers are almost inevitable among diabetic patients. They occur because a diabetic neuropathic foot is much more fragile and therefore susceptible to injuries from friction, and from the weight of your entire body. Sometimes, injected insulin increases the chances of foot ulcers.
Most Diabetic patients have had a foot ulcer at least once. It is a common occurrence, but exercise, proper diet, and hygiene can reduce their occurrences and also keep your neuropathy under control. To make sure foot ulcers never become anything serious, proper care and hygiene is a must. Make sure your feet are always clean and dry. Sweat accumulation can not only cause foot ulcers but also infections, which due to neuropathy, can go unnoticed. If you have sweaty feet, make sure you wash your feet with a mild soap and pat dry each foot.
Wearing sturdy shoes outdoors and protective socks indoors is also a must. They will give you the right amount of protection from injuries and reduce the chances of foot ulcers. But not all socks are appropriate for diabetic neuropathic patients. In the section below we will look at Syounaa Socks and the role they play in managing your diabetic neuropathy.
Syounaa Socks And Diabetic Neuropathy
Though it varies from patient to patient, many would feel a difference within a week of tying out Syounaa. Unlike other diabetic socks that are simply padded at the heals, Syounaa socks are made with Celliant Technology. The Celliant fibers used to manufacture our socks have 13 safe, naturally occurring, thermo-reactive minerals infused within them. These minerals trap body heat and convert it into infrared energy. The socks emit the recycled energy back to our body to promote blood circulation, increase blood oxygen and stimulate tissue in the foot. As a result, patients feel reduced pain and irritation. The increased supply of oxygen reduces the number of blisters that surface on our skin and also reduce mild numbness.
Though the socks only cover the foot and lower calf area, it provides benefits to your entire leg. By facilitating blood flow on your feet, it reduces pressure from your calves and thighs as well. Unlike other diabetic socks, Syounaa Therapeutic socks can decrease the chances of foot amputations, ulcers, and infections.
Diabetic feet need to be clean and dry all the time. This is especially important if you have diabetic neuropathy because you cannot rely on your natural senses of touch. With regular socks and shoes, you have a lot more chances of sweat accumulation. Syounaa socks, on the other hand, are made with a special sweat absorbent feature. It absorbs the sweat within its fabric and keeps it away from your body so that you can stay clean and dry. Syounaa socks are ideal for working individuals who have to travel every day and can’t change their socks frequently. Clean dry feet are safer and much more protected from infection.
After a long day, make sure to wash these socks along with other clothes. Washing the socks do not affect its efficacy. Avoid handling the fabric as much as possible and only wear it after it is completely dry. This will help you maintain clean and healthy feet and protect you from infections.
Keeping diabetic patients in mind Syounaa socks are designed without an elastic band at the rim. If you see regular socks they have an elastic band that secures the sock in place. Though it is a cost-effective feature that poses no threat to non-diabetic patients, those suffering from diabetic neuropathy face serious consequences. The elastic band cuts the oxygen supply in the place that is most crucial for the peripheral diabetic neuropathic patient and worsens the condition. Syounaa socks ensure that your feet are not deprived of oxygen and therefore does not have an elastic band to keep it in place.
You may wonder how the socks stay in place if they don’t have an elastic band. Syounaa socks are form fitting, which means that they take the shape of your feet without suffocating it. It almost fits like extra skin – one that removes pressure from your feet feels comfortable and lets them breathe.
The exercise tips we mentioned above will be most effective if they are done in Syounaa socks. Rotating your feet and exercising your calf muscles will stimulate blood flow and Syounaa socks will alleviate pressure from your feet so that you can exercise for longer. The excess warmth around your feet will allow the socks to trap the moisture and prevent it from escaping the body. It will be emitted back to your body at a later time.
After working out with Syounaa socks, you may notice yourself having longer, more successful training sessions. You may be able to hold your balance for longer or have enough stamina for more reps. This happens because the Celliant fiber used in the socks, allow for more blood flow around your feet and remove pressure from them. Higher blood flow leads to more oxygenation and when our legs have an increased supply of oxygen we automatically start performing better. So, don’t be surprised if you see a sudden shift in endurance levels.
After a good workout, remember to take off your socks and put them for the wash. Wash your feet thoroughly with a mild soap and dry it completely before wearing a clean pair of Syounaa socks. This is especially important if you have sweat intensely during a workout session.
You may be wondering about the side effects. The truth is there are no side effects. It may be hard to believe but the minerals used are naturally occurring and there are no chemicals or harmful additions to the fabric. The socks work with body heat which is a natural form of energy. Body heat is emitted back to the body and no one has side effects on his or her own body heat.
In rare cases, an individual may show an allergic reaction to the cloth fabric or to any one of the 13 minerals used in the socks. So far, there haven’t been any cases of allergic reactions towards Syounaa Socks.
When Should You Wear Syounaa Diabetic Socks
To get the best results from Syounaa socks, make sure to wear them for as long as possible. You may have to change them in the day if you accumulate too much sweat around your feet or after an intense workout session.
Syounaa socks can be work during:
- Walking
- Jogging
- At home
- At work
- While travelling
- While sleeping
- During exercise
What Are The Advantages Of Syounaa Diabetic Socks?
Protects your feet from friction rubs, blisters, and ulcers
- Cushions your feet and prevents it from injuries
- It is shape confirming not constricting. This means that it takes up the shape of your feet without suffocating it
- Made to control odour and prevent infection around the feet
- Owing to its’ shape confirming nature, it does not wrinkle or cause any discomfort
- Provides mild compression for better circulation
- Does not contain tight elastic fibres like regular socks and hence does not cut blood circulation at the lower calf area
- Reduces the chances of foot injuries and amputation
• Protects sensitive pressure points

Conclusion
Diabetic Neuropathy can be extremely painful and peripherical diabetic neuropathy is usually the most common kind of neuropathy caused by diabetes. Though the condition is not reversible, proper care and treatment can slow down the damage caused by this condition. In this article, we have discussed a little about the condition, neuropathy, how it occurs, how to prevent it or reduce the pain in neuropathy and how Syounaa socks help in this condition.
More than 60% diabetic patients may have mild or severe forms of neuropathy and the chances of getting this condition increase as the years go by. So, a person who has been diabetic for more than 20 – 25 years is much more likely to get diabetic neuropathy. Never ignore symptoms of pain, numbness or tingling sensations. There have been past cases where patients learned of their diabetes only after being diagnosed with diabetic neuropathy. These symptoms may be subtle indications of diabetic neuropathy. A doctor will help you indicate the severity of the condition so the sooner you book an appointment, the better.
With proper care, we can keep both our diabetes and diabetic neuropathy under control. Syounaa Socks take a step further. They take care of your feet, reduce pain and numbness so that you can carry on with the rest of your life.
